Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Symptoms and Complications of Influenza a in the Elderly Upon arrival at the Hospital
*Corresponding author:Dalibor Sedláček, Department of Infectious Diseases and Travel Medicine, Faculty of Medicine in Pilsen, Charles University, Faculty Hospital Pilsen, Czech Republic.
Received:November 28, 2022; Published:December 13, 2022
DOI: 10.34297/AJBSR.2022.17.002379
Abstract
Influenza A and B viruses cause epidemics every year, with approximately 3–5 million serious cases and about 300 thousand deaths worldwide. Most patients die from bacterial complications of influenza. The authors studied the course, laboratory findings, complications and causes of death in a set of 261 patients over the age of 65, of whom 218 were hospitalized and 43 were treated in an outpatient setting. Typical flu symptoms included fever, cough, general weakness, fatigue, myalgia, arthralgia, headache and chills. Patients who later developed complications had elevated values of CRP, procalcitonin, urea and creatinine. Of the bacterial agents, Klebsiella pneumoniae and Streptococcus pneumoniae were most often involved in complications. The antiviral drug oseltamivir was administered to 226 of 261 seniors. 47 (18.01%) people died from influenza and its complications. The causes were severe pneumonia with acute respiratory insufficiency and severe heart failure. As an effective prevention of the development of diseases and complications, the authors recommend annual timely vaccination, optimally with a tetravalent influenza vaccine.
Introduction
Influenza is an infectious disease caused by influenza viruses A and B, which belong to the family of orthomyxoviruses. Viruses belong to the genus of influenza viruses. The rarer influenza virus C then forms a completely separate special genus. Influenza A and B viruses are responsible for epidemics each year, with approximately 3–5 million serious cases and about 300,000 deaths worldwide [1]. The European Centre for Disease Control estimates that influenza causes more than 38,000 deaths in Europe every year [2]. Mortality is not significantly different when affected by influenza A and B. It is approximately 16% for the former and about 10% for the latter [3]. Most patients die from complications of influenza. A more common complication of influenza is bacterial pneumonia. Bronchitis and sinusitis can also occur in the airway area. Dangerous complications of influenza can also concern the heart, mainly myocarditis and pericarditis. Up to 90% of pericarditis in developed countries are idiopathic, which could be related to a viral disease [4]. Normally, exacerbations of various chronic diseases (COPD, bronchial asthma, chronic heart failure and others) can be observed as a complication.
Material & Methods
A retrospective analysis of patient data was performed. The monitored group consisted of all patients over 65 years of age, who were diagnosed with influenza in the period between 1 January 2018 and 31 December 2020 at all workplaces of the University Hospital in Pilsen on the basis of anamnesis, clinical picture and subsequent virological examination. Retrospectively, data from the electronic medical records of patients in the WinMedicalc program (Medicalc Software, s. r. o., Plzeň, Czech Republic) were obtained. We monitored the anamnesis and nature of the difficulties, symptoms at the initial examination, laboratory results, results of microbiological examinations, complications and the final condition. We also noted flu vaccination information. Prior to processing, data anonymization was carried out. The data was processed in the Excel 2016 spreadsheet editor (Microsoft Corporation, Redmond, USA). Statistical processing was carried out using the PROGRAM STATISTICA (StatSoft CR, s. r. o., Prague, Czech Republic). The local ethics committee was informed prior to the start of data collection and, due to the nature of the study, no approval or informed consent of patients was required.
Results
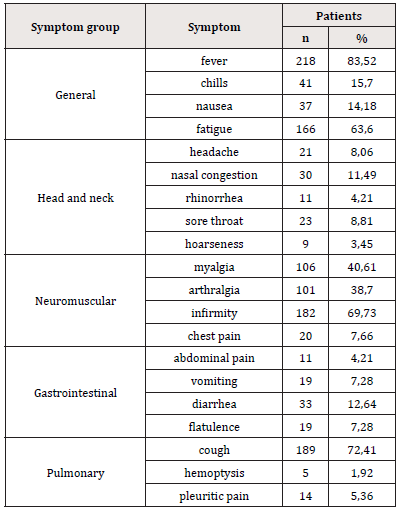
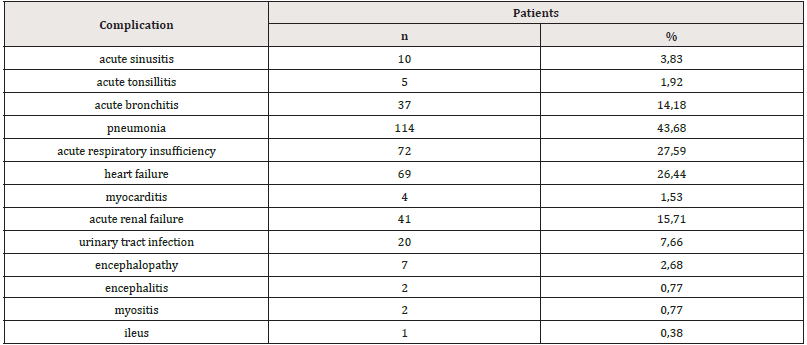
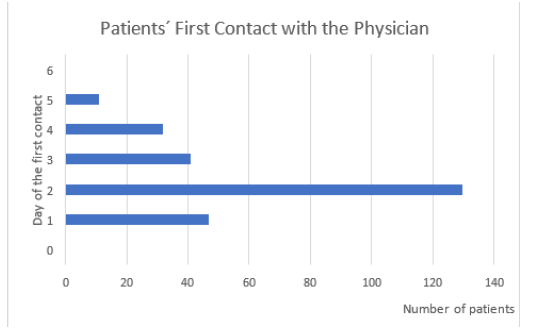
In the study period, the diagnosis of influenza A was confirmed in 602 patients. Of these, 261 were seniors (43.36%), 286 patients (47.51%) were of working age and 55 were children (9.13%). There were 143 women and 118 men in the senior group. The average age was 77.48 years, the median being 76 years, with a minimum of 65 years and a maximum of 99 years. The maximum number of diagnosed flu illnesses in the elderly was during the month of February. Of the 261 patients over 65 years of age, only 43 were treated on an outpatient basis, all without risk factors and complications, and 218 were hospitalized. Of the 218 seniors hospitalized, 163 (74.77%) were treated in a standard bed, 40 (18.35%) required a stay in a first- or second-degree intensive care bed, and 15 patients (6.88%) required higher-level resuscitation care in a third-degree intensive care bed. From the point of view of the patient’s first contact with the doctor from the onset of symptoms, the largest group consisted of seniors who were examined by the doctor on the 3rd day from the onset of symptoms. There were 121 patients (46.36%) of 261. The interval from the onset of difficulties to the first medical examination is shown in Figure 1. The most common symptoms of influenza in the elderly were fever in 218 cases (83.52%). Cough occurred in 189 seniors (72.41%). Fever and cough combined occurred in 160 cases (61.3%). Other more common symptoms included reported general weakness in 182 (69.73%) and fatigue in 166 elderly patients (63.6%). 106 patients (40.61%) suffered from myalgia, while 101 patients (38.7%) suffered from arthralgia. Headache was reported by only 21 patients (8.06%) in the senior population. At baseline, 41 patients (15.7%) reported chills. The incidence of flu symptoms in patients in our set is shown in Table 1. In blood counts, the mean leukocyte count at the first blood draw was 9.23 × 109/L, erythrocytes 4.31 × 1012/L and platelets 188.14 × 109/L. The mean value in seniors with an uncomplicated course was 51 mg/L, in patients with complications 90.79 mg/L. Procalcitonin levels were determined in only 147 of the 261 patients. Of these, the average value for patients without complications was 0.33 mg/L and for complicated seniors 1.73 mg/L. By default, urea and creatinine levels were monitored. In patients without complications, values were within the limits of normal, but in patients with complications of influenza disease the mean values of urea were 11.2 mmol/L and creatinine was 126.59 mmol/L. In the whole set, the average values of sodium in the ionogram were 138.95 mmol/L, chloride was 101.54 mmol/L and potassium was 4.0 mmol/L. No complications were observed in 69 seniors in the group. 192 (73.56%) experienced a diverse range of complications. 114 seniors of the whole group (43.68%) developed pneumonia, the etiology of which was demonstrated in 48 cases. Most often these were the bacteria Klebsiella pneumoniae and Streptococcus pneumoniae. 69 cardiac patients of older age experienced acute cardiac decompensation. Acute respiratory insufficiency was diagnosed in 72 patients (27.59%). Of these, 49 received sufficient oxygen therapy with a mask or nasal spikes with a higher oxygen flow, 8 were connected to HFNO, 5 temporarily required non-invasive lung ventilation in an intensive care bed, and another 10 had to have secured airways by tracheal intubation and artificial lung ventilation. Acute renal impairment was confirmed in 41 patients (15.71%). In addition to pneumonia, we diagnosed acute bronchitis in 37 cases. In 14 patients, we observed an exacerbation of chronic obstructive pulmonary disease. Another more common infectious complication of influenza, outside the respiratory tract, was a urinary tract infection that occurred in 20 patients (7.66%) of our total population. An overview of complications of influenza in our patient population is shown in Table 2. Antiviral treatment with oseltamivir was indicated in 226 of the 261 seniors (86.59%) of our population. Other antiviral drugs effective against influenza viruses were not used. Demonstrably, only 11 seniors in whom the disease was confirmed were vaccinated against influenza; an effective prevention of the development of the disease. Hospitalization was necessary in 6 of them because there were complications within the respiratory system. Neither of these patients died. 105 patients were found not to be vaccinated, in the remaining 145 seniors the information about the flu vaccination cannot be traced back in the medical records. Of the 261 seniors, 47 died from influenza and its complications (18.01%). Most of these patients developed severe pneumonia with acute respiratory insufficiency. In some patients, severe heart failure occurred simultaneously or independently. One patient developed acute colitis followed by an ileous condition. Decompensation of other chronic diseases of patients in older age was usually observed.
Discussion
Seniors are one of the risk groups at high risk for complications of influenza, which is why annual vaccination is recommended for them [5-7]. The symptoms of influenza in the elderly are different and concern, as in adults of working age and in children, the respiratory and digestive tract, the musculoskeletal system. We also observe the classic, general symptoms of a viral disease. These often include fever, cough, myalgia, breathing-dependent chest pain, headache, sore throat and chills [8-10]. Most often, however, fever and cough occur directly [11]. The results of our study confirm this. Fever occurred in 83.52% and cough in 72.41% of seniors. Together, these symptoms occurred in 61.3%. However, some results show that in the elderly, fever and cough have a significantly lower predictive value for influenza than in the adult population of working age [12]. Some authors point out that in seniors we may encounter an absence of fever and only mild systemic symptoms more often than in young adults, but qualitative changes in consciousness are more common [13,14]. More often we can also encounter only fever and impaired consciousness, especially if pneumonia occurs at the same time as a complication of influenza disease [15]. In general, it is necessary to state that at the time of increased incidence of influenza, an automated system for measuring body temperature at the entrance to an urgent reception can increase the detection of patients with this disease. An increase in the number of people caught with elevated body temperature correlates with an increased incidence of influenza in a given region [16]. Even during the flu season, one should not forget about the possibility of contracting the SARS-CoV-2 virus. Covid-19 co-infection with influenza has been repeatedly documented. It is more common in elderly patients or people with other risk factors [17,18]. Accurate and early diagnosis of influenza is essential for the elderly, as they are at risk of developing serious complications [19,20]. The most common complications include pneumonia, invasive bacterial co-infection, myositis and exacerbation of chronic diseases [21]. Chronic diseases include cardiovascular diseases, chronic respiratory diseases, renal, hepatic and hematological diseases [22]. Even in our group of patients, we observed pneumonia as the most common complication. This occurred in 43.68% of seniors. Influenza viruses themselves can cause severe pneumonia, however, mortality is significantly increased mainly by secondary bacterial pneumonia [23]. This is the case in normal epidemic occurrences, and it has been even more pronounced in most pandemics in documented history [24-26]. The most common pathogen causing bacterial pneumonia in influenza disease is Streptococcus pneumoniae [27-29]. Staphylococcus aureus, including MRSA [30], is also more frequently reported. In our study, we detected the bacteria Klebsiella pneumoniae and Streptococcus pneumoniae the most. Among the most common complications we observed acute bronchitis, exacerbation of chronic respiratory diseases and acute respiratory insufficiency in the respiratory tract. Not infrequently, acute cardiac decompensation occurred as a complication. We also often observed acute deterioration of kidney function, sometimes of a higher degree, which is a commonly described, not rare, complication of influenza disease [31]. Laboratory findings were in no way out of line with common findings in respiratory viral diseases. Mostly leukocytosis was observed in the blood count. The level of C reactive protein was also consistent with the findings in common viral infections.
Procalcitonin reliably indicated possible bacterial complications of influenza.
A side finding of our study is the fact that interleukin-6 is not commonly examined in our hospital in flu patients, although it is a significant predictor of the severity of influenza disease and its further development [32], as is the case, for example, with covid-19 [33,34]. The interval of the first contact with the doctor from the beginning of the symptoms of the disease was often decisive for the further prognosis of the patient. On the first day of difficulties, no patient sought medical help. In the interval of 2-5 days from the beginning of the onset of symptoms, 96.43% of patients came to the university hospital, the rest came on the 6th day of persistent difficulties. Lam [11] reports that in the group of elderly patients studied by him, 54% visited the emergency department 2-5 days after the onset of symptoms. Even later, 29% of elderly patients did so. We consider it important to state that all patients over 65 years of age who died of influenza and its complications in the teaching hospital in the monitored period came into contact with the doctor no earlier than on the 3rd day after the onset of the difficulties. In our group, 226 out of 261 seniors (86.59%) were treated with oseltamivir. It was usually administered twice daily, orally, at a dose of 75 mg. In no case was the possible development of resistance to oseltamivir observed in the literature [35,36]. Normally, patients were not corticosteroids, as many studies have shown an increase in mortality [37-39], a greater number of complications [40,41] and a prolonged release of the influenza virus [42].
Conclusion
Seniors are a group of fragile patients with many chronic diseases and smaller reserves of the organism. The most common symptoms, and thus the predictors of the disease, during the flu season are mainly the rapid onset of fever and dry cough. Influenza in the elderly is often accompanied by many complications.
These are pneumonia, exacerbation of chronic diseases of the respiratory and cardiovascular systems, liver disease, impaired renal function and myositis. In our group of patients, pneumonia was the most common. Acute heart failure and impaired renal function were also treated more often. Mortality in our population reached 18.01%. The most effective prevention of the development of influenza and its complications is the available vaccination with a tetravalent vaccine, which contains an inactivated split virus of four strains of influenza A and B.
References
- Simons L (2004) Pandemic influenza and mortality: past evidence and projections for the future. Board on Global Health. The Threat of Pandemic influenza: Are We Ready? The National Academies Press. pp.432.
- Preaud E, Durand L, Macabeo B, Norbert Farkas, Brigitte Sloesen, et al. (2014) Annual public health and economic benefits of seasonal influenza vaccination: a European estimation. BMC Public Health 14: 813- 824.
- Asai N, Yokoi T, Nishiyama N, Yusuke Koizumi, Daisuke Sakanashi, et al. (2017) Secondary organizing pneumonia following viral pneumonia caused by severe influenza B: a case report and literature reviews. BMC Infect Dis 17(1): 572.
- Maisch B, Seferovic PM, Ristic AD, Raimund Erbel, Reiner Rienmüller, et al. (2004) Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J 25(7): 587-610.
- Gao H, Lu H, Cao B, Hong Shang, Jian-He Gan, et al. (2013) Clinical Findings in 111 Cases of Influenza A (H7N9) Virus Infection. N Engl J Med 368(24): 2277-2285.
- Ghebrehewet S, MacPherson P, Ho A (2016) Influenza. BMJ 355: i6258.
- Rolfes MA, Flannery B, Chung J, Alissa O Halloran, Shikha Garg, et al. (2019) Effects of Influenza Vaccination in the United States during the 2017–2018 Influenza Season. Clin Infect Dis 69(11): 1845-1853.
- Pitigoi D, Lupulescu E, Alexandrescu V (2009) Effects of Influenza Efficiency of seasonal influenza vaccine in persons older than 65 in Romania. Pilot case-control study I-MOVE, 2008-2009. Bacteriol Virusol Parazitol Epidemiol 54: 109-116.
- Savulescu C, Valenciano M, de Mateo S, Larrauri A (2010) Estimating the influenza vaccine effectiveness in elderly on a yearly basis using the Spanish influenza surveillance network Pilot case-control studies using different control groups, 2008–2009 season, Spain. Vaccine 28(16): 2903-2907.
- Shahid Z, Kleppinger A, Gentleman B, Ann R Falsey, Janet E McElhaney, et al. (2010) Clinical and immunologic predictors of influenza illness among vaccinated older adults. Vaccine 28(38): 6145-6151.
- Lam PP, Coleman BL, Green K, Jeff Powis, David Richardson, et al. (2016) Predictors of influenza among older adults in the emergency department. BMC Infect Dis 16(1): 615.
- Govaert TME, Dinant GJ, Aretz K (1998) The predictive value of influenza symptomatology in elderly people. Fam Pract 15(1): 16-22.
- Walsh EE, Cox C, Flasey AR (2002) Clinical features of influenza A virus infection in older hospitalized persons. J Am Geriatr Soc 50(9): 1498-1503.
- Monmany J, Rabella N, Margall N, P Domingo, I Gich, et al. (2004) Unmasking influenza virus infection in patients attended to in the emergency department. Infection 32(2): 89-97.
- Falsey AR, Walsh EE (2006) Viral pneumonia in older adults. Clin Infect Dis 42(4): 518-524.
- Bordonaro SF, McGilicuddy D, Pompei F, Charles Harding, Leon D Sanchez, et al.(2016) Human temperatures for syndromic surveillance in the emergency department: data from the autumn wave of the 2009 swine flu (H1N1) pandemic and a seasonal influenza outbreak. BMC Emerg Med 16: 16.
- Brenner EJ, Ungaro RC, Gearry RB, Gilaad G Kaplan, Michele KH, et al. (2020) Corticosteroids, But Not TNF Antagonists, Are Associated with Adverse COVID-19 Outcomes in Patients with Inflammatory Bowel Diseases: Results From an International Registry. Gastroenterology 159(2): 481-491.
- Jing R, Vunnam RR, Schnaubelt E David Goldner, Srinivas Rao Vunnam, Chad Vokoun, et al. (2021) Co-infection of COVID-19 and influenza A in a hemodialysis patient: a case report. BMC Infect Dis 21(1): 68.
- Schanzer DL, Langley JM, Tam TW (2008) Role of influenza and other respiratory viruses in admissions of adults to Canadian hospitals. Influenza Other Respi Viruses 2(1): 1-8.
- Lang PO, Mendes A, Socquet J, Noémie A, Sheila G, et al. (2012) Effectiveness of influenza vaccine in aging and older adults: comprehensive analysis of the evidence. Clin Interv Aging 7: 55-64.
- Jani AA, Uyeki TM (2018) Emergency management of infectious diseases. (2nd edn), Cambridge University Press, Cambridge, UK,
- Grohskopf LA, Sokolow LZ, Broder KR, Emmanuel BW, Alicia MF, et al. (2017) Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices – United States, 2017-2018 influenza season. MMWR Recomm Rep 67(3): 1-20.
- Kash JC, Taubengerger JK (2015) The role of viral, host, and secondary bacterial factors in influenza pathogenesis. Am J Pathol 185(6): 1528-1536.
- Morens DM, Taubengerger JK, Fauci AS (2008) Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis 198(7): 962-970.
- Weinberger DM, Simonsen L, Jordan R, Steiner C, Miller M, et al. (2012) Impact of the 2009 influenza pandemic on pneumococcal pneumonia hospitalizations in the United States. J Infect Dis 205(3): 458-465.
- Tognotti E (2009) Influenza pandemics: A historical retrospect. J Infect Dev Ctries 3(5): 331-334.
- McNamee LA, Harmsen AG (2006) Both Influenza-Induced Neutrophil Dysfunction and Neutrophil-Independent Mechanism Contribute to Increased Susceptibility to a secondary Streptococcus pneumoniae Infection. Infect Immun 74(12): 6707-6721.
- Short KR, Habets MN, Hermans PWM, Dimitri AD, et al. (2012) Interactions between Streptococcus pneumoniae and influenza virus: a mutually beneficial relationship? Furture Microbiol 7(5): 609-624.
- Ishiguro T, Kojima A, Shimizu T, Norikatsu M, Seiichiro K, et al. (2019) Combined hemophagocytic syndrome and thrombotic microangiopathy due to mixed infection with influenza virus and pneumococcal pneumonia. Clin Case Rep 7: 131-134.
- Dawood FS, Chaves SS, Perez A, Arthur R, James M, et al. (2014) Complications and associated bacterial coinfections among children hospitalized with saesonal or pandemic influenza, United States, 2003-2010. J Infect Dis 209(5): 686-694.
- Bagshaw SM, Sood MM, Long J, Robert AF, Neill KJ Adhikari, et al. (2013) Acute kidney injury among critically ill patients with pandemic H1N1 influenza A in Canada: cohort study. BMC Nephrol 14: 123.
- Zhang J, Wang J, Gong Y, Yudan G, Qiangqiang X, et al. (2022) Interleukin-6 and granulocyte colony –stimulating factor as predictors of the prognosis of influenza-associated pneumonia. BMC Infect Dis 22(1): 343.
- Tjendra Y, Al Mana AF, Espejo AP, Yamac A, Nicolas CM, et al. (2020) Predicting Disease Severity and Outcome in COVID-19 Patients: A Review of Multiple Biomarkers. Arch Pathol Lab Med 144(12): 1465-1474.
- Gao Y, Li T, Han M, Xiuyong L, Dong W, et al. (2020) Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol 92(7): 791-796.
- Baz M, Abed Y, Papenburg J, Xavier B, ME Hamelin, et al. (2009) Emergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxis. N Engl J Med 361(23): 2296-2297.
- Roussy JF, Abed Y, Bouhy X, Guy Boivin (2013) Emergence of an oseltamivir resistant influenza A/H3N2 virus in an elderly patient receiving a suboptimal dose of antiviral prophylaxis. J Clin Microbiol 51(12): 4234-4236.
- Han K, Ma H, An X, Yang S, Jing C, et al. (2011) Early use of glucocorticoids was a risk factor for critical disease and death from pH1N1 infection. Clin Infect Dis 53(4): 326-333.
- Delaney JW, Pinto R, Long J, François L, Neill KA, et al. (2016) The influence of corticosteroid treatment on the outcome of influenza A (H1N1pdm09) – related critical illness. Crit Care 20: 75.
- Li H, Yang SG, Gu L, Y Zhang, XX Yan, et al. (2017) Effect of low-to-moderate-dose corticosteroids on mortality of hospitalized adolescents and adults with influenza A(H1N1) pmd09 viral pneumonia. Influenza Other Respir Viruses 11(4): 345-354.
- Linko R, Pettilä V, Ruokonen E, S Karlsson, J Tenhunen, et al. (2011) Corticosteroid therapy in intensive care unit patients with PCR-confirmed influenza A(H1N1) infection in Finland. Acta Anaesthesiol Scand 55(8): 971-979.
- Lee N, Leo YS, Cao B, Paul KS Chan, WM Kyaw, et al. (2015) Neuraminidase inhibitors, superinfection and corticoides affect survival of influenza patients. Eur Respir J 45(6): 1642-1652.
- N Lee, CS Cockram, PK S Chan, DS C Hui, KW Choi, et al. (2008) Antiviral treatment for patients hospitalized with severe influenza infection may affect clinical outcomes. Clin Infect Dis 46(8): 1323-1324.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.